Eye Care
What should happen during an exceptional eye examination?
A comprehensive eye examination should consist of a number of different tests. First of all, the doctor should take time to visit with the patient and get to know them well in order to best understand his or her needs. Exceptional eyecare can greatly enhance the quality of an individual's life and improve his or her efficiency at work, during recreational activities, and at home.
Initial Testing
A thorough eye examination should include an assessment of the patients' visual acuity (reading the eye chart). This gives the doctor an idea of how well the patient is seeing before any tests are performed.
There are six eye muscles that control each eye. The doctor should ask the patient to follow a target into six primary positions of gaze to ensure that each eye muscle is working properly. This test also helps the doctor determine the range of eye muscle movement and balance to verify that the eyes are straight and working together as a team.
Measuring the Shape of the Eye
To measure the shape of the eye, a test called Keratometry or Topography is performed to determine the size and shape of the surface lens of each eye. This gives the doctor information regarding the patient's prescription, whether or not the patient has astigmatism, and the health of the anterior lens of the eye (the cornea). In order to get a perfect fit for contact lenses, this test is absolutely necessary. This measurement allows the doctor to ensure that the size and shape of the contact matches the size and shape of the lens on the surface of the eye. Even a slight mismatch in this measurement can decrease the comfort and clarity of a contact lens.
Measuring the Internal Pressure of the Eye - Glaucoma
After measuring the eye, Tonometry should then be performed to measure intra-ocular pressure (the pressure inside of the eye). This can be done by a skilled doctor using a variety of instruments. One of these instruments blows a puff of air at the eye. This method is generally one of the tests that patients dislike because it is startling. In recent years, new "soft puff" tonometers have been developed that are significantly more patient friendly. We acquired a "soft puff" tonometer some time ago, and patients have appreciated this addition. If a patient would prefer to have the pressure measured using a different instrument that does not emit a puff of air, we can easily and happily accommodate such a request.
Elevated intra-ocular pressure can be a sign of glaucoma. Glaucoma is a potentially blinding disease where elevated pressure causes damage to the optic nerve resulting in loss of vision. The challenging aspect in treating glaucoma is that there are no symptoms to the disease. For many patients, glaucoma is effectively treated with one eye drop a day. Annual eye examinations are essential to the diagnosis, treatment, and subsequent preservation of vision for a patient with glaucoma. Vision loss due to glaucoma is a preventable tragedy that generally only occurs when patients are not examined regularly.
Should any sign of glaucoma be present, other tests will be performed during a second visit. These tests include a visual field examination, pachymetry (which measures the thickness of the lens of the eye), and fundus photography (taking several pictures of the inside of the eye). These, and other additional tests, require special instruments that we have here in our office. The information that these tests provide, allows the doctor to make crucial decisions regarding the diagnosis and management of patients who are at risk for glaucoma.
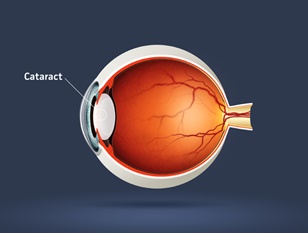
Health Evaluation of the Anterior Eye - Cataracts
To gain a detailed evaluation of the eye, biomicroscopy should be performed using a special microscope called a biomicroscope or slit lamp. This microscope allows the doctor to examine the individual structures of the eye in great detail. First, the eyelids and eyelashes are examined. The cornea (the clear lens on the surface of the eye) is examined next. This examination is especially important for patients who wear contact lenses. If the contact lens is not fit correctly or if the patient does not care for his or her contacts in an appropriate manner, the patient can develop swelling in the cornea or blood vessels that grow from the white part of the eye (sclera, conjunctiva) onto the cornea. If these changes to the health of the eye are not recognized and managed, a patient's ability to wear contact lenses can be affected.
The iris (the colored part of the eye) is also examined with the biomicroscope. The crystalline lens is the second lens of the eye and sits behind the iris. This lens is not normally visible to the naked eye. As the body matures, this lens which is clear, transparent, and flexible as a child, will harden, turn yellow, and become more opaque. This process occurs naturally as we age, and is sped up by ultra violet light exposure. When this lens yellows to a certain level it becomes a cataract and will cause poor vision.
Dr. Wilkes examines the eyes for cataracts, and when a patient is diagnosed with a cataract, he will monitor the growth of a cataract through an annual exam. When the cataract progresses to a certain level, Dr. Wilkes will refer the patient to one of the many fine surgeons he works with for a cataract removal. The decision to monitor or refer the cataract is based on the appearance and severity of the cataract, and the symptoms experienced by the patient.
Evaluating the visual system
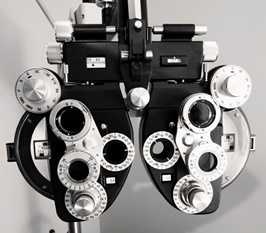
The prescription of the patient is evaluated using a phoropter. A phoropter is the instrument that the patient looks through while the doctor changes lenses to evaluate the visual system of the patient. This process should consist of more than simply asking the patient "which is more clear lens number one, or lens number two". There are additional tests that can and should be performed to determine how the eyes balance and move when looking through a given prescription. Many doctors no longer do these types of tests, but we believe that these tests allow us to prescribe a prescription that provides more natural vision. These additional tests only take five extra minutes, but are essential in determining which contact lens or eyeglass prescription will make the patient the most happy and comfortable.
Dr. Wilkes may also put some lenses in a trial frame to match your prescription. Measuring a prescription is a stationary test, and yet human beings move around during the day. Sometimes, a prescription that feels comfortable when a patient is seated in a dark room holding still, is not the most comfortable prescription once the patient starts moving around and engaging in their everyday activities. Trial framing a prescription allows the patient to test drive their new vision prior to receiving their final prescription for spectacles or contact lenses.
Health Evaluation of the Inside of the Eye - Macular Degneration
A comprehensive eye examination should include ophthalmoscopy. Ophthalmoscopy is the process through which the eye doctor examines the retina. The doctor will get close to you and look in your eye to perform this test. Dr. Wilkes may also dilate the patient's pupils and use several other microscopes (one of which he wears on his head with a light on it) to examine the peripheral retinal. The retina lines the inside of the eye like an inner tube inside of a tire. It has special cells called rods and cones which absorb light and send a signal back to the brain through the optic nerve. This signal is then registered in the brain as vision.
The retina is very thin, much thinner than cellophane and is subject to certain diseases. The retina can develop holes in it through the natural thinning process that occurs as we age, or when the eye or head is bumped or jarred. If fluid leaks under the retina through one of these holes, the retina can detach from the inside of the eye (retinal detachment). If this occurs, vision will be lost wherever the retina is not touching the inside of the eye. When Dr. Wilkes finds a hole or detachment in the retina, he refers the patient to one of several fine retinal specialists he works with in the area to repair the problem.
The leading cause of blindness in Americans over the age of 70 is macular degeneration. Macular degeneration is a buildup of sun damaged cells in the central area of the retina called the macula. There are two types of macular degenarion, dry and wet.
Dry macular degeneration occurs when the cells in the macula (central area of the retina) are damaged from years of absorbing ultra violet light. One of the best protections against macular degeneration is the wearing of lenses that protect the eye from ultra-violet light. A diet high in green leafy vegetables, and foods that contain omega-3 fatty acids are also beneficial in protecting the eye against macular degeneration. Most people, if they live long enough, will develop some form of macular degeneration. The better our diet is and the more we protect our eyes from ultra violet light, the older we will be before we develop macular degeneration. Dry (atrophic) macular degeneration is a slow buildup of sun damaged cells (drusen) in the central area of the retina. This is the most common type of macular degeneration and will result in a slow loss of the fine detail in our central vision.
Wet macular degeneration (exudative) occurs when abnormal blood vessels grow underneath the surface of the macula (the central area of the retina, responsible for fine detailed vision). These blood vessels are weak, and can easily leak or burst. If these blood vessels burst, the retina is severely damaged and vision loss occurs. Regular eye examinations allow Dr. Wilkes to monitor the retina for development of theses blood vessels. If wet macular degeneration is found, Dr. Wilkes will refer the patient to a retinal specialist who can administer an injection, and in many cases, stop the blood vessels before they can cause irreversible damage.
Diabetes & High Blood Pressure - What else can be seen in an eye examination?
The eye is one of the only places in the body where blood vessels can be seen without cutting any tissue. Consequently, vascular diseases like diabetes and high blood pressure can be seen in the eye. Diabetic retinopathy is one of the leading causes of blindness. Patients who are diabetic or who have a history of high blood pressure or thyroid disease should have their eyes examined and dilated at least every year. More frequent examinations should be given if the eye doctor feels it is necessary.